Should test your gut microbiome?
Share
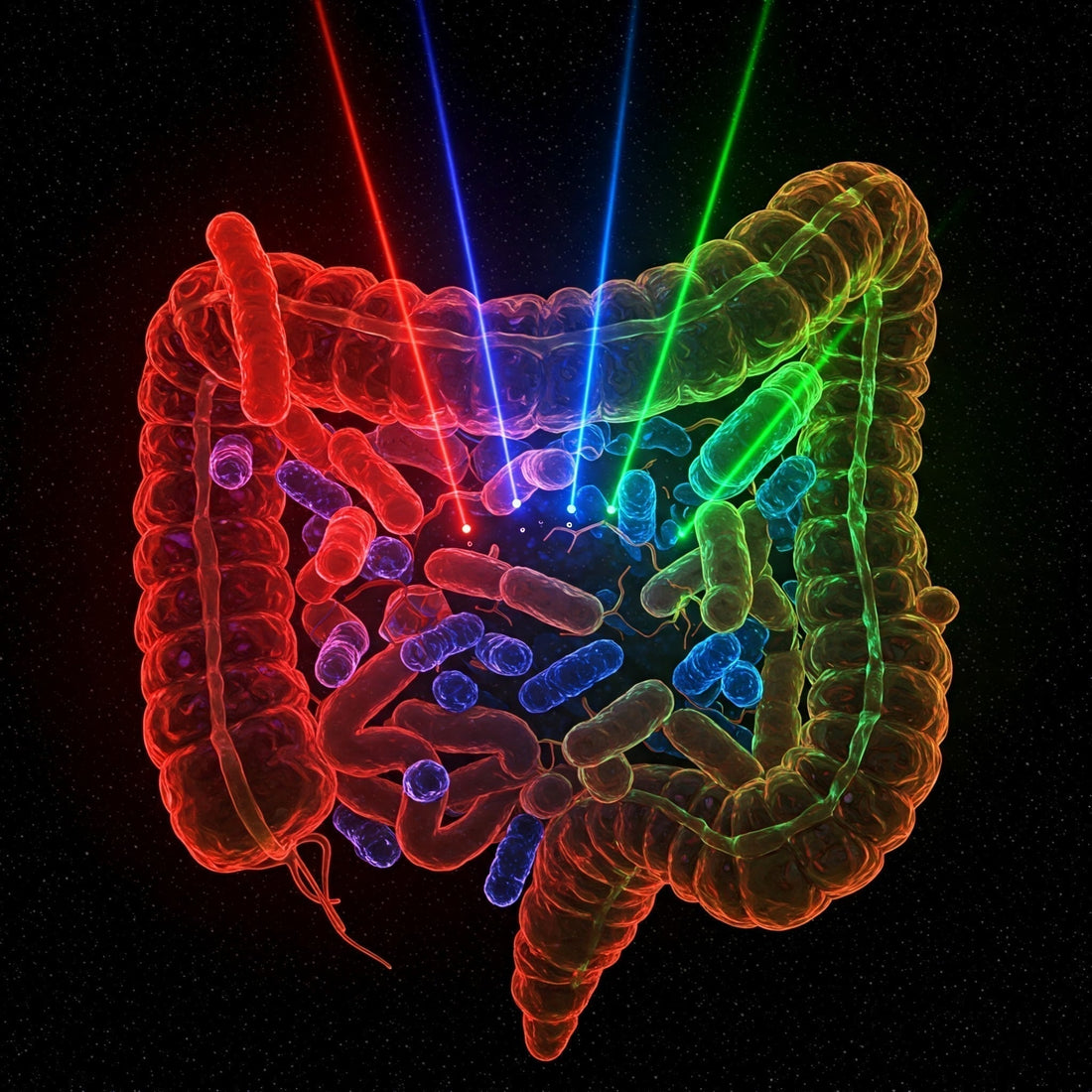
The gut microbiome—a complex community of microorganisms residing in our digestive tract—plays a pivotal role in maintaining our overall health. Its influence spans from aiding digestion to modulating the immune system and even impacting mental well-being. However, defining what constitutes a "healthy" gut microbiome remains a subject of ongoing scientific exploration. Microbiome tests have exploded in popularity in recent years, but are they worthwhile?
Challenges in Defining a Healthy Gut Microbiome
In their comprehensive review, Van Hul et al. (2024) delve into the intricacies of characterising a healthy gut microbiome. They highlight several challenges:
-
Individual Variability: Each person's gut microbiome is unique, influenced by factors such as genetics, diet, environment, and lifestyle. This variability complicates the establishment of a universal standard for gut health.
-
Dynamic Nature: The gut microbiome is not static; it evolves over time in response to various stimuli, including dietary changes, medications, and illnesses. Capturing a single, representative snapshot of a healthy microbiome is, therefore, challenging.
-
Functional Redundancy: Different microbial species can perform similar functions within the gut ecosystem. This redundancy means that a healthy microbiome might not depend on specific microbial compositions but rather on the overall functional capacity of the microbial community.
-
Causation vs. Correlation: Determining whether changes in the gut microbiome cause certain health conditions or are a result of them remains a complex endeavor. This bidirectional relationship complicates our understanding of the microbiome's role in disease.
Markers of a Healthy Gut Microbiome
Despite these challenges, researchers have proposed several indicators that may signify a healthy gut microbiome. These measures can be found by measuring the composition (diversity), functional capacity and resilience of the gut microbiome.
1. Measuring Composition (Diversity)
A diverse microbiome is often associated with resilience and stability, potentially contributing to better health outcomes.
Specific phyla of bacteria, such as the Bacillota/Bacteroidota ratio have been pointed to as a potential indicator for health. This is because Bacillota may be more efficient at extracting energy from food, leading to weight gain. A higher ratio is therefore associated with being less healthy. A high Bacillota/Bacteroidota ratio has also been linked to several diseases such as inflammatory bowel disease and irritable bowel syndrome. Despite this, there is still conflicting evidence across several studies, testament to the complexity of interacting factors in the gut microbiome.
Enterotypes have also been discovered, categorising individuals based on the predominant microbial communities within their guts. This can give a correlation-based indication of disease risks. On its own though, the concept of enterotypes may oversimplify the complex and dynamic nature of the gut microbiome, which is
influenced by numerous factors, including diet, environment and genetics.
2. Measuring Functionality
Beyond composition, the ability of the microbiome to perform essential functions, such as producing beneficial metabolites like short-chain fatty acids, is crucial. Functional diversity—the range of functions performed by the microbiota—might be more suited to evaluate the continued proper operation of the gut ecosystem. Strangely, a high species diversity in the gut microbiome does not always translate into a high functional diversity.
There is a lot of functional redundancy within the gut microbiome - meaning that the same species can perform the same functions. This means that functional biomarkers of activity may provide a more accurate representation of the health of the gut microbiome. Afterall, it's the function the microbes perform that matters, rather than just their presence.
The problem with this approach is that its mega-expensive, necessitating metagenomics and bioinformatics. Even if we did this for everyone, the functionalities vary so much between individuals, more research is needed to figure out what this all means.
3. Measuring Resilience
A healthy microbiome can maintain or quickly return to its original state after disturbances, such as antibiotic use or dietary changes. Measuring this over the long-term could give clues about the overall health of the gut microbiome.
The Path Forward: Personalised Approaches
Given the complexities and individual differences, Van Hul et al. advocate for personalised approaches to defining and achieving gut health. They emphasise the need for:
-
Longitudinal Studies: Tracking individuals' microbiomes over time to understand changes and identify patterns associated with health and disease.
-
Standardised Methodologies: Developing consistent protocols for microbiome research to enable comparability across studies.
-
Holistic Assessments: Considering diet, lifestyle, genetics, and environmental factors alongside microbiome analyses to gain a comprehensive understanding of gut health.
In conclusion, some measures of microbiome composition can provide some insight into the health of the microbiome. With this said, it's important to take results with a pinch of salt, as it's not the whole story. Complexity in the environment, genetics, and diet affect the microbiome, and thus the useful of testing it.
Reference: Van Hul, M., Cani, P.D., Petitfils, C., De Vos, W.M., Tilg, H. and El-Omar, E.M., 2024. What defines a healthy gut microbiome?. Gut, 73(11), pp.1893-1908.
